By Sam Dunklau, WITF.
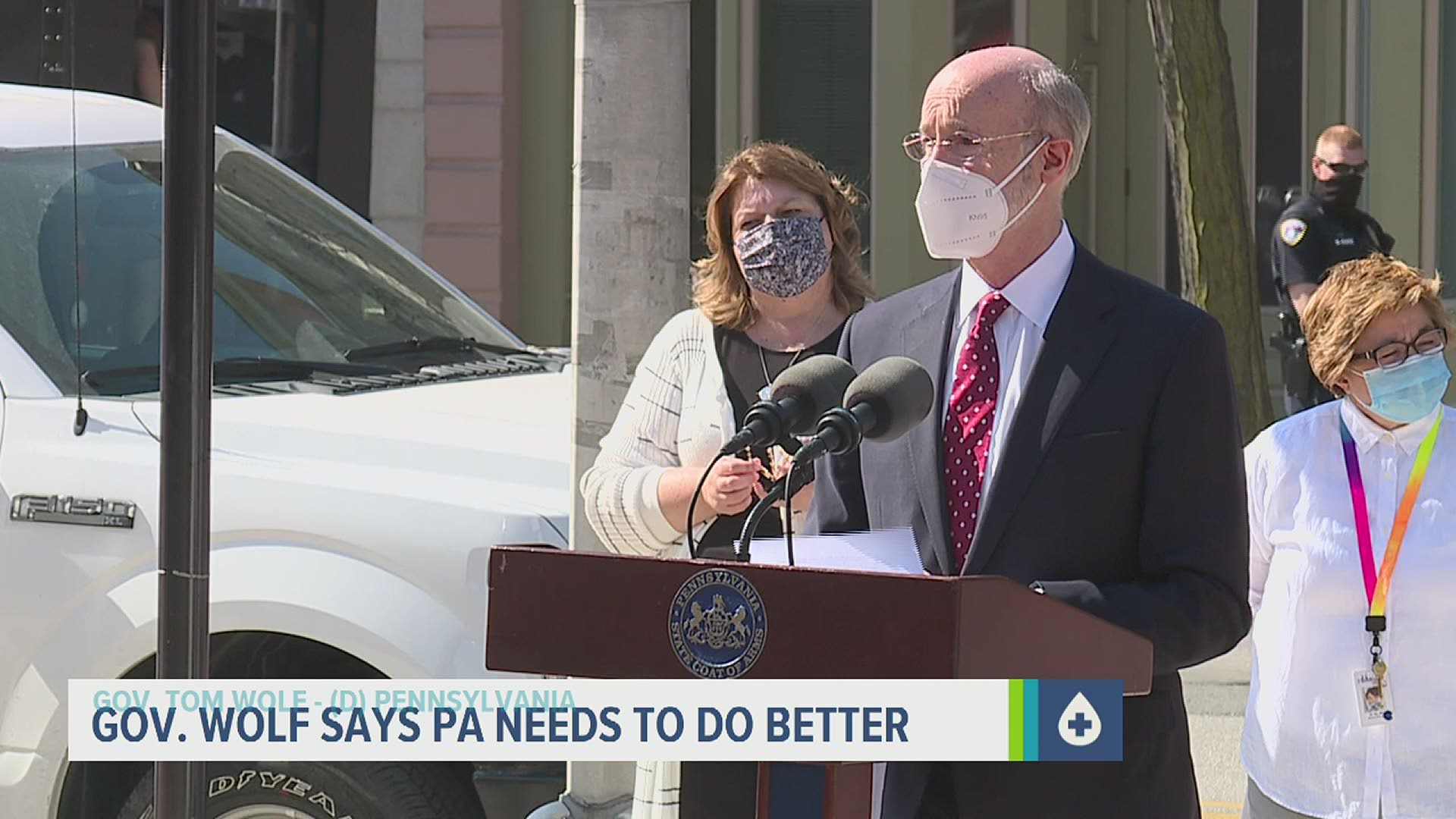
Gov. Tom Wolf received a first dose of the Moderna vaccine at a community health center in York Monday morning. He joins more than four million Pennsylvanians who have gotten a first dose since the state began vaccinating people against the coronavirus in December.
Wolf said he made the appointment last Tuesday, the day the commonwealth opened vaccine eligibility to all adults. For months, health workers had only been allowed to vaccinate people over the age of 65, those with certain underlying health conditions, and essential workers most at-risk of catching the disease.
“I wanted to wait in line,†Wolf said after his 15-minute observation period was up. “I made my appointment and this was the appointment.†When asked how he was feeling in the first minutes after his vaccine, Wolf responded, “Great.â€
All states were to have opened vaccine appointments to all adults this week, if they hadn’t already. So far, children under 16 are not eligible for a shot in Pennsylvania. Earlier this month, the nation’s top infectious disease expert Dr. Anthony Fauci told reporters there could be enough child safety data from clinical trial by the end of the year. That means kids may be able to get shots by then, if the vaccination doses are considered safe for them.
Wolf said outside of child eligibility, the next big hurdle his administration plans to tackle is vaccine hesitancy.
“Until this past week, the issue was inadequate supply. Now, we’re just starting to get to the point where we have open appointments in a lot of places all around the commonwealth. So, it’s time to really start focusing on the [the] hesitancy issue,†Wolf said.
Dr. Asceline S. Go administered Wolf’s vaccine and serves as the Vice President of Medical Services at the York City clinic. She said fears about rare blood clots caused by the Johnson & Johnson vaccine have already led some to cancel their vaccine appointments at the facility in the last week.
Regulators are set to determine whether the J&J jab can continue with new guidance this week. Only six patients reported such clotting out of nearly 7 million people in the U.S. who received that vaccine.
Go said workplace incentives and more mobile vaccination drives could help reduce access barriers and get those who are holding out more comfortable with rolling up their sleeves.
“There is a lot of work that needs to be done, and it has to be a cooperation among the leaders of the community,†Go said. “If there’s no reason for them not to get the vaccine, then the chance of them getting it would exponentially be higher.â€
Wolf said the commonwealth is ramping up its own plans to target hesitant communities with public service ads. The New York Times reports counties where a majority voted for former President Donald Trump in the last election are seeing lower vaccination rates on average.